Can Anyone Develop Lung Cancer? Understanding Risks Beyond Smoking
Lung cancer can affect anyone—even those who have never smoked. Understanding hidden risks is the first step toward prevention and early detection.
When most people think of lung cancer, they picture someone who has smoked for years. But the truth is, tens of thousands of people who never smoked are diagnosed with lung cancer every year. Understanding why this happens—and what you can do to lower your risk—can save lives.
Smoking Isn’t the Only Cause
Smoking remains the leading cause of lung cancer—but it’s not the only one.
Smoking remains the biggest risk factor for lung cancer, responsible for about 80% to 90% of lung cancer deaths in the United States.
But doctors and researchers now know that 10% to 20% of lung cancers occur in people who have never smoked—that’s between 20,000 and 40,000 Americans each year.
So, what’s causing lung cancer in people who’ve never touched a cigarette? Several hidden risks play a role.
Radon: The Silent Threat at Home
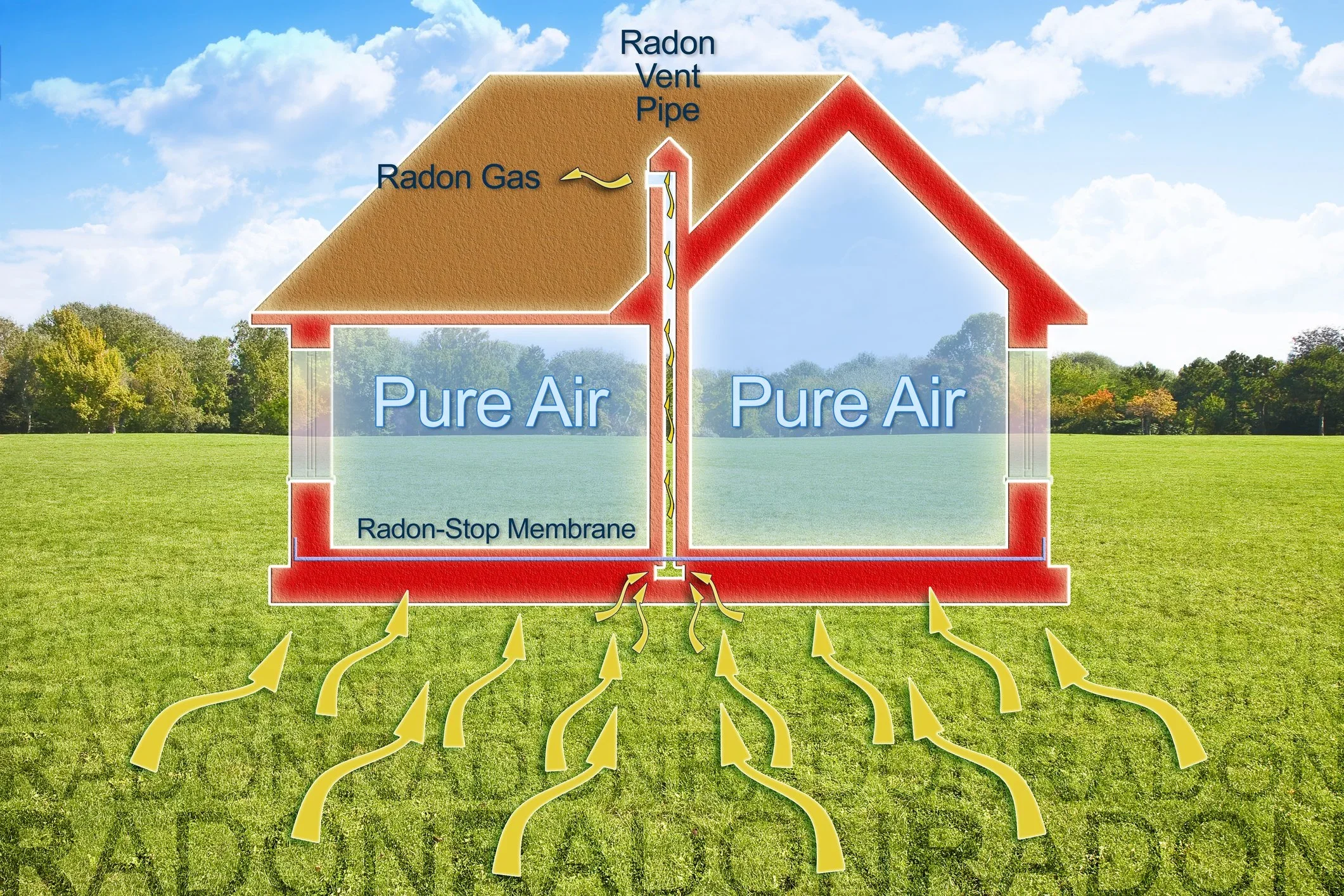
Diagram illustrating how radon gas seeps from the ground into homes and can accumulate without proper ventilation.
Radon is a colorless, odorless gas that naturally seeps from rocks and soil. When it builds up indoors—especially in basements or lower floors—it can be dangerous.
According to the Environmental Protection Agency (EPA), radon is the leading cause of lung cancer among people who don’t smoke, contributing to thousands of deaths every year.
The good news? You can test your home for radon with an inexpensive kit and fix any problems with proper ventilation.
Learn more about how radon exposure contributes to lung cancer risk and how to protect your home here.
Secondhand Smoke Exposure
Secondhand smoke exposure, even in enclosed spaces like cars, increases a non-smoker’s risk of lung cancer.
Even if you don’t smoke, being around someone who does can harm your lungs. Breathing in other people’s smoke—called secondhand smoke—increases a non-smoker’s risk of lung cancer by about 30%.
Each year, secondhand smoke causes roughly 7,300 lung cancer deaths among U.S. adults who have never smoked.
Air Pollution and Workplace Hazards
Long-term exposure to fine particles from industrial emissions and workplace hazards increases lung cancer risk, even in non-smokers.
The air we breathe also matters. Long-term exposure to air pollution—especially fine particles from traffic and industrial emissions—has been linked to lung cancer in never-smokers.
A 2022 NIH study found that tiny particles in polluted air can trigger genetic mutations that lead to cancer.
People who work with asbestos, diesel exhaust, or other industrial chemicals are also at higher risk, even if they’ve never smoked.
Learn how wildfire smoke exposure increases lung cancer risk and what early detection options are available here.
Family History and Genetics
Family history can influence lung cancer risk, highlighting the importance of awareness and early screening for loved ones.
Sometimes, the risk comes from within. Around 8% of lung cancers are linked to inherited or familial factors.
If a close relative has had lung cancer, your chances may be higher—especially when combined with other risks like pollution or past exposure to secondhand smoke.
A Rising Trend Among Never-Smokers
Lung cancer among never-smokers is becoming more common. Studies show that the share of lung cancer in people who never smoked has nearly doubled over the past two decades, now making up about 15% of cases in the U.S.
Interestingly, it’s more common in women than men and often diagnosed at a younger age than smoking-related lung cancer.
Lung cancer among younger adults and non-smokers is on the rise. Discover why in our article Too Young for Lung Cancer? The Truth May Surprise You.
Prevention and Early Detection Save Lives
Regular checkups and early detection tests—like Cizzle Bio’s CIZ1B blood test—can dramatically improve treatment outcomes.
You can’t control every risk, but you can take steps to protect yourself:
Test your home for radon (especially if you live in older or basement-level housing).
Avoid secondhand smoke—ask smokers to step outside.
Limit exposure to chemicals or fumes at work by following safety guidelines.
Get regular checkups and talk to your doctor if you have a cough, chest pain, or shortness of breath that won’t go away.
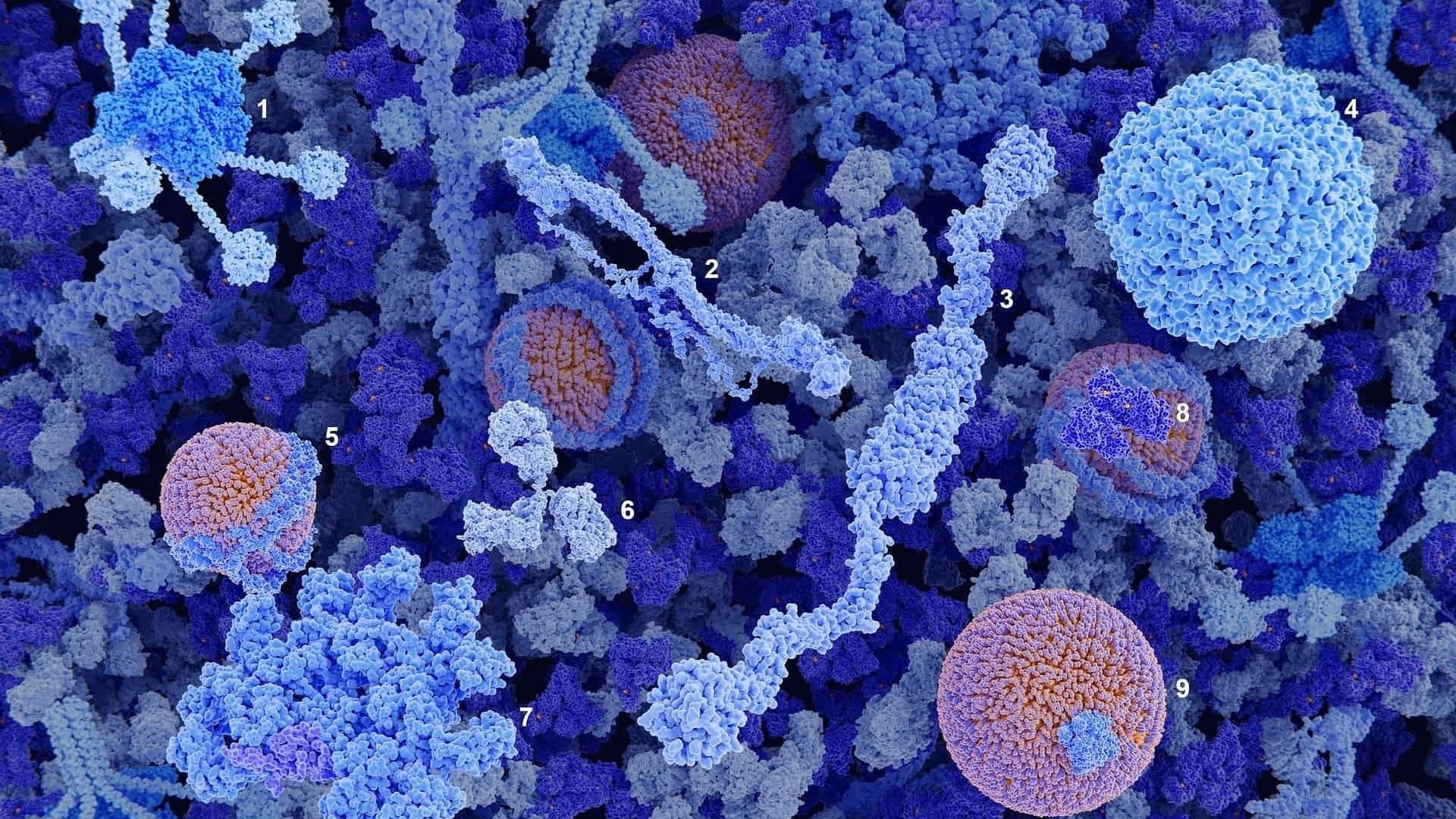
Early detection is key. Biomarker-based blood tests, like Cizzle Bio’s CIZ1B test—coming soon to U.S. healthcare providers—are designed to find lung cancer in its earliest, most treatable stage. Many people live with lung cancer for years before symptoms appear—find out why here. Detecting cancer early gives patients more treatment options and can raise survival rates dramatically.
Learn more about how early detection improves survival outcomes in our article, Early Detection and Lung Cancer Survival: The Difference It Makes.
Discover how blood-based biomarkers like CIZ1B are transforming early lung cancer detection in Blood-Based Biomarkers: The Future of Lung Cancer Detection.
For a full overview of current screening methods and eligibility criteria, read our Comprehensive Guide to Lung Cancer Screening.
The Takeaway
Anyone can develop lung cancer—even if they’ve never smoked.
By understanding the hidden risks, taking preventive steps, and supporting advances in early detection, we can save more lives and give everyone a better chance at a healthy future.
For more information about Cizzle Bio’s CIZ1B biomarker blood test for early lung cancer, please visit: www.cizzlebio.com
Sources
Centers for Disease Control and Prevention (CDC), 2024 – Lung Cancer Risk Factors
Environmental Protection Agency (EPA), 2024 – Health Risk of Radon
National Institutes of Health (NIH), 2025 – Air Pollution and Lung Cancer Risk
American Cancer Society (ACS), 2024 – Lung Cancer Causes and Prevention
Hackensack Meridian Health, 2023 – Understanding Lung Cancer Risks
JAMA Oncology, 2021 – Trends in Lung Cancer Among Never-Smokers













Stomach cancer is one of the deadliest cancers worldwide, but catching it early can significantly improve survival. Learn which risk factors to watch for, what symptoms should not be ignored, and how Cizzle Bio’s DEX-G2 biomarker blood test may help detect gastric cancer sooner, when treatment works best.