Lung Cancer Screening Rates are Still Too Low—The CIZ1B Biomarker Blood Test Could Help Save Thousands More Lives
Lung cancer remains the deadliest cancer in America and globally. Yet new research shows that tens of thousands of lives could be saved each year if more people were screened—and if screening guidelines were expanded to reach those at risk who are falling through the cracks.
Today, fewer than 1 in 5 eligible adults receive lung cancer screening. And when screening doesn’t happen, lung cancer is often found late, when treatment is harder, more expensive, and less effective.
Two new national studies published in JAMA and JAMA Network Open show how large this missed opportunity is—and why it’s time to rethink how we screen for lung cancer. They also underscore how more accessible options, including low-cost, minimally invasive biomarker blood tests like CIZ1B, could remove major barriers that keep people from getting screened.
Only 18.7% of People Get Screened for Lung Cancer
Researchers from the American Cancer Society analyzed data and found:
Only 18.7% of eligible adults are up to date on lung cancer screening
Current screening rates prevent just 24% of potential lung cancer deaths
With full uptake, screening could prevent 62,110 deaths over five years—more than four times the current impact
If everyone who qualifies got screened, more than 60,000 additional lives could be saved by 2030.
The study also showed that states vary widely—some with screening rates as low as 9%, other no higher than 31%. This gap leaves thousands of patients undiagnosed until symptoms appear, often when the disease is advanced and has spread to other parts of the body.
Screening Guidelines Miss Most Lung Cancer Cases
A second study from Northwestern University examined nearly 1,000 lung cancer patients and found that current U.S. Preventive Services Task Force (USPSTF) criteria capture only a fraction of real-world cases.
Key findings include:
Only 35.1% of lung cancer patients met current screening criteria
Universal age-based screening (age 40-85) would detect 93.9% of cancers
Expanding older guidelines would still miss almost 40% of cancers
Many left out of current criteria are women; Asian and other minority groups; and never-smokers who still developed slung cancer
At least 26,124 deaths could be prevented annually under an age-based model
The study clearly shows—tobacco-based criteria miss too many people who go on to develop lung cancer. Lung cancer is no longer only a “smoker’s disease,” and our screening must reflect this.
Why Screening Rates are Low
Low-dose CT (LDCT) scans—the current standard for screening—save lives. But many patients avoid screening because:
They are worried about radiation exposure
They lack easy access to imaging centers
The eligibility rules are confusing
They don’t think they qualify
They feel healthy and put off screening
The tests require scheduling, travel, and time off work
How a Simple Blood Test Like CIZ1B Could Expand Early Detection
When the screening process is complex, people are far less likely to participate—and cancers go undetected until symptoms appear.
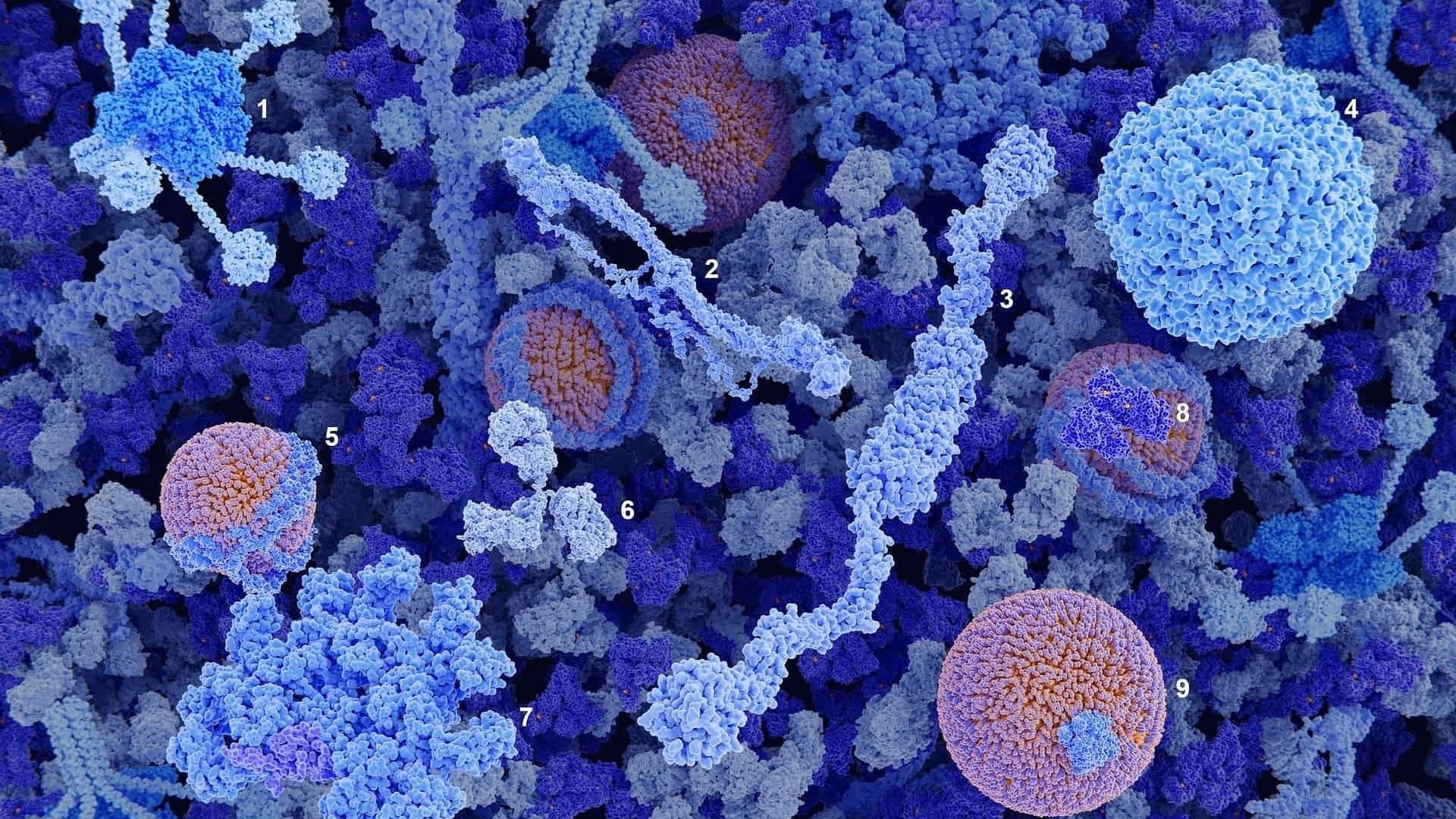
A biomarker blood test such as CIZ1B offers a more accessible approach to early lung cancer detection. Because it requires only a routine blood draw—less than a tablespoon of blood—CIZ1B can:
Expand screening access for people who avoid CT scans or live far from image centers
Reach people not covered by current screening guidelines, including light smokers, former smokers, never-smokers, or those with environmental exposures
Remove common barriers such as fear of radiation or complicated rules
Increase participation rates, helping find more cancers at earlier, more treatable stages
The Research is Clear—Lung Cancer Screening Saves Lives
Both studies show that major gains in survival come from detecting more cancers early. A simple, minimally invasive biomarker blood test such as CIZ1B can bring screening to people who might otherwise never be tested.
With screening rates under 20% and current guidelines missing most diagnoses, tests such as CIZ1B can play a powerful role in reaching more people, expanding screening beyond current criteria, and finding lung cancers at earlier, more treatable stages.
Cizzle Bio is committed to advancing diagnostic solutions that make early detection the global standard of care.
To learn more about our groundbreaking CIZ1B biomarker blood test—coming soon to U.S. healthcare providers—please visit:
Sources
MEDPAGETODAY, 2025 - More Lung Cancer Screening Could Prevent Over 60,000 U.S. Deaths by 2030
MEDPAGETODAY, 2025 - Current Lung Cancer Screening Guidelines Miss Most Tumors, Study Suggests












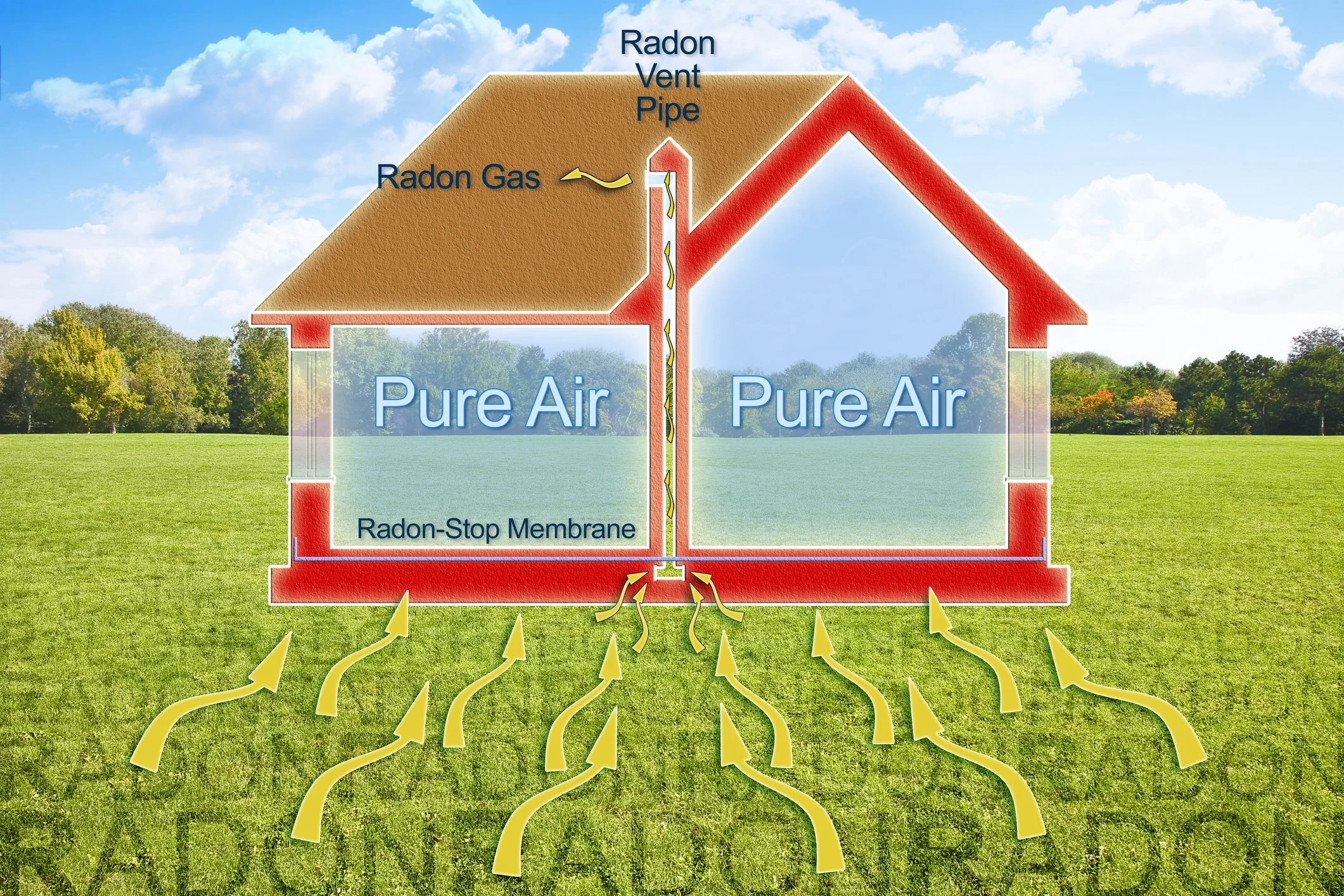









Lung cancer is often linked to a mix of risk factors, some preventable and others environmental. Learn the leading causes, what you can do to reduce exposure, and when screening may be appropriate.