Key Causes of Lung Cancer—Why Knowledge Leads to Power
Lung cancer doesn’t have one single cause but is often linked to a combination of risk factors that build over time. Some are preventable, others are environmental or inherited, and many go unnoticed.
Understanding what increases your lung cancer risk matters because awareness supports earlier action. Knowledge can help you reduce exposures where possible, recognize when your risk may be higher than you realized, and start conversations with your clinician sooner about whether lung cancer screening is right for you.
Tobacco Smoke—the Leading Risk Factor
Cigarette smoking and secondhand smoke exposure cause nearly 9 out of 10 lung cancer deaths. ¹ Secondhand smoke also increases lung cancer risk, even for people who have never smoked. ²
What You Can Do
If you smoke, ask your clinician about evidence-based cessation support. ¹
If you don’t smoke, reduce secondhand smoke exposure when possible, especially at home and in cars. ²
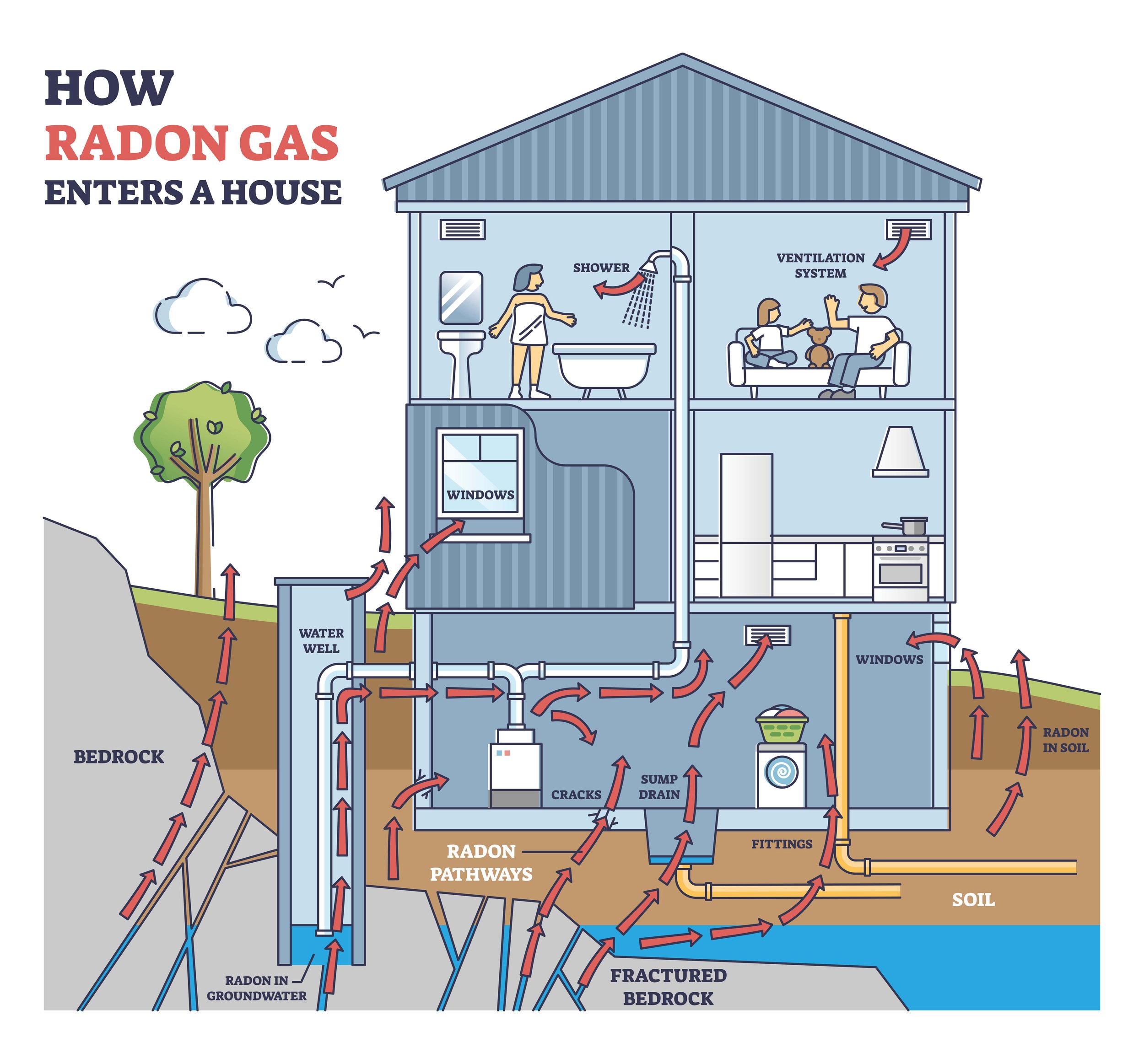
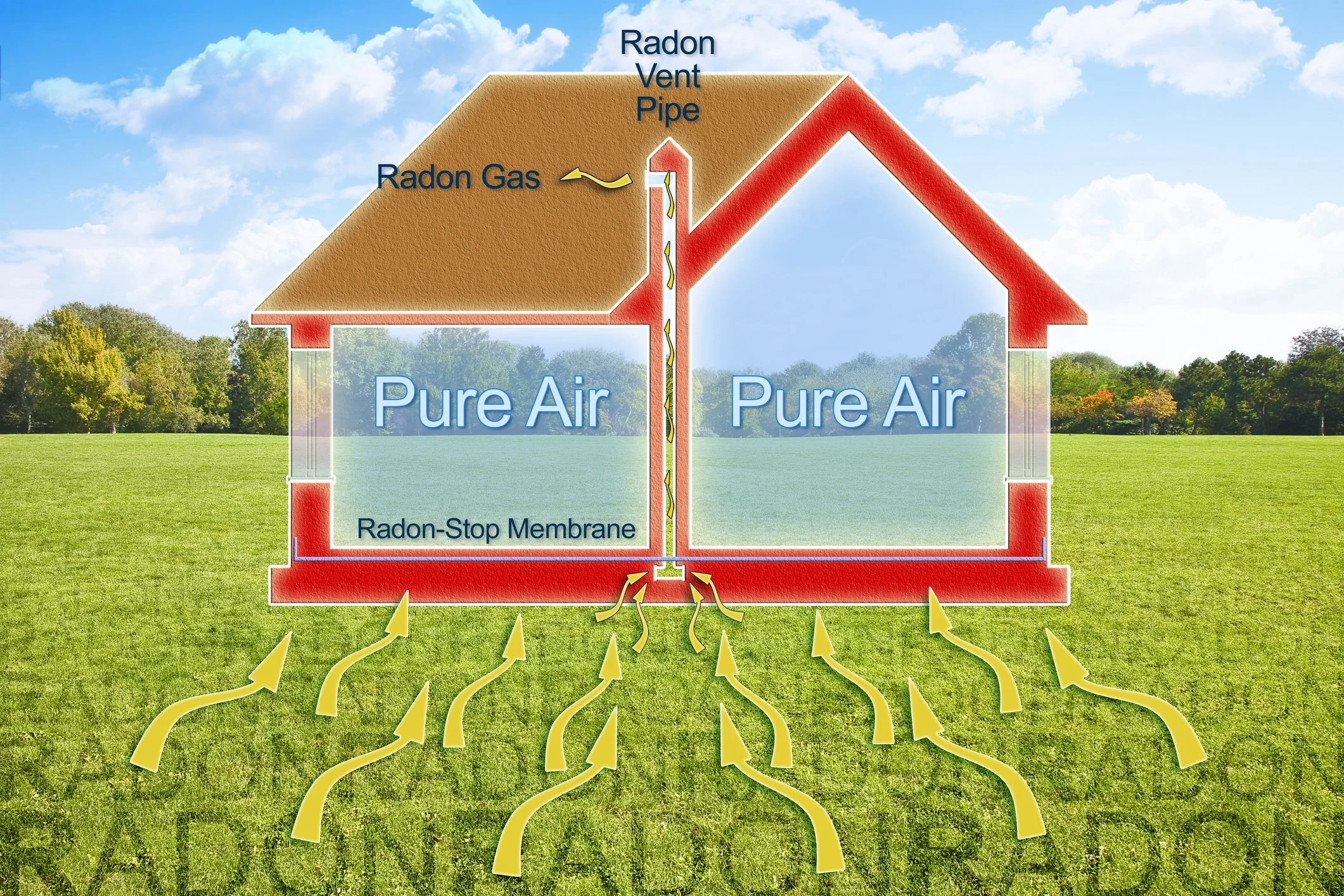
Radon—An Invisible Risk That Can Build Up Indoors
Radon is a naturally occurring radioactive gas that can be present indoors. It is the number one cause of lung cancer among non-smokers and the second leading cause overall. ³
What You Can Do
Test your home for radon because testing is the only way to know your home’s radon level. ³
If your level is high, take steps to reduce it through mitigation. ³
Workplace Exposures and Outdoor Air Pollution
Lung Cancer Can Occur in People Who Never Smoked
It’s important to understand that lung cancer is not limited to smokers. In the United States, about 10% to 20% of lung cancers, or 20,000 to 40,000 each year, happen in people who never smoked or smoked fewer than 100 cigarettes in their lifetime. ⁶
What You Can Do
If you have concerns, talk with your clinician about your risk factors, even if you have never smoked. ⁶
Stay aware of your environment, including secondhand smoke, radon, diesel exhaust, and other air pollution. ⁶
Screening and Early Action
Early detection can lead to better outcomes for those with lung cancer. And for people at higher risk, screening may help identify lung cancer earlier, when treatment options are more effective and lives can be saved.
The U.S. Preventive Services Task Force recommends annual low-dose CT (LDCT) screening for adults ages 50 to 80 with at least a 20 pack-year smoking history who currently smoke or quit within the past 15 years. ⁷ If you are unsure whether you qualify, your clinician can help you decide. ⁷
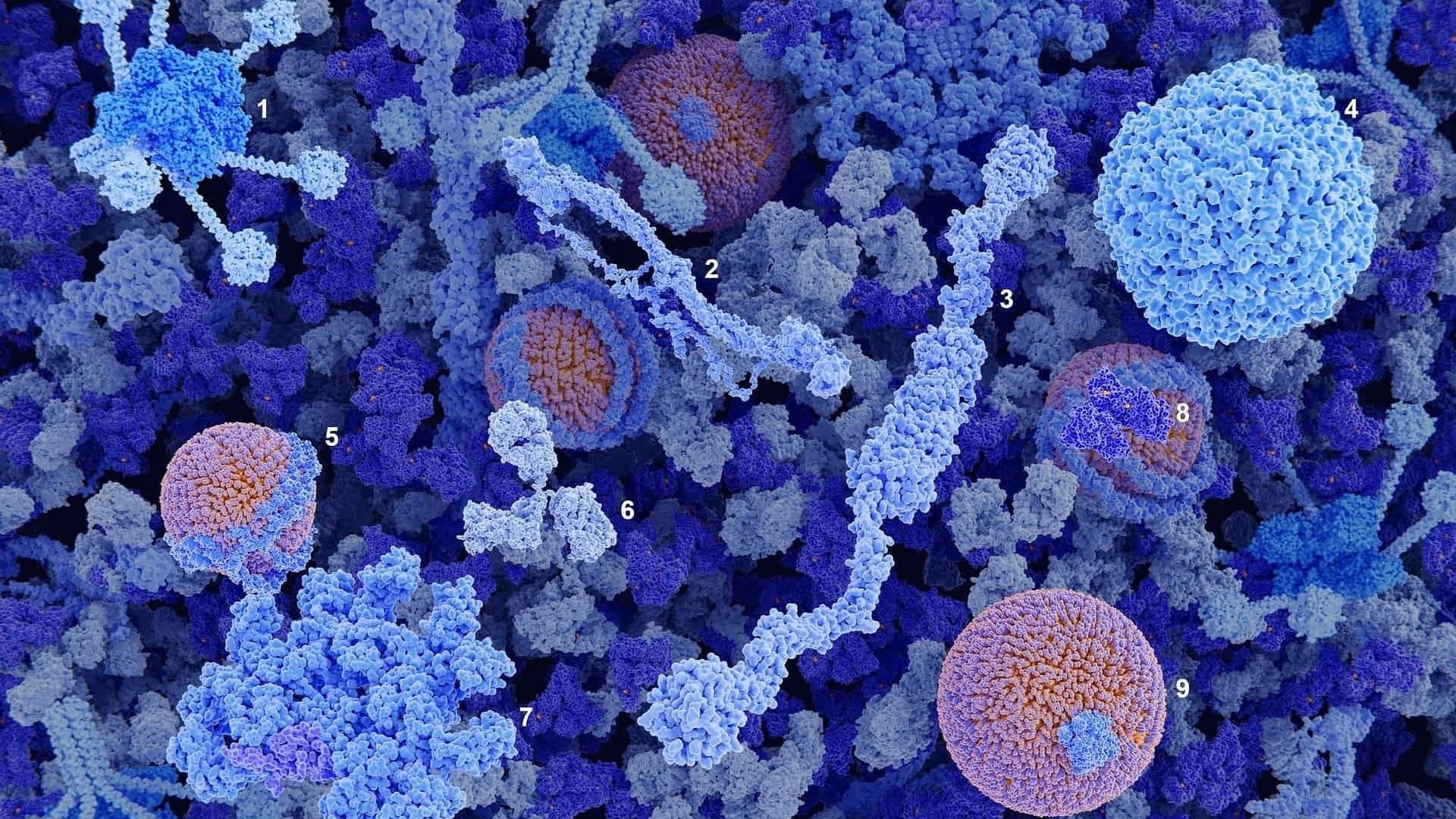
The Power of Early Detection with CIZ1B
At Cizzle Bio, we know that early detection saves lives. Our groundbreaking biomarker blood test, CIZ1B, is designed to help identify lung cancer earlier, when treatment options are more effective. ⁸ Using less than a tablespoon of blood, this simple but powerful blood test can provide lifesaving answers.
CIZ1B will soon be available to U.S. healthcare providers. To learn more, please visit: www.cizzlebio.com. ⁸
This article is for educational purposes and does not provide medical advice. If you have symptoms or concerns, please contact a licensed healthcare professional.
References (AMA)
Centers for Disease Control and Prevention. Health Effects of Cigarettes: Cancer. Updated September 17, 2024. Accessed January 13, 2026. https://www.cdc.gov/tobacco/about/cigarettes-and-cancer.html
Centers for Disease Control and Prevention. Health Problems Caused by Secondhand Smoke. Updated January 31, 2025. Accessed January 13, 2026. https://www.cdc.gov/tobacco/secondhand-smoke/health.html
US Environmental Protection Agency. Health Risk of Radon. Accessed January 13, 2026. https://www.epa.gov/radon/health-risk-radon
Centers for Disease Control and Prevention. Lung Cancer Risk Factors. Updated February 13, 2025. Accessed January 13, 2026. https://www.cdc.gov/lung-cancer/risk-factors/index.html
Turner MC, Andersen ZJ, Baccarelli A, et al. Outdoor air pollution and cancer: an overview of the current evidence and public health recommendations. CA Cancer J Clin. 2020;70(6):460-479. doi:10.3322/caac.21632
Centers for Disease Control and Prevention. Lung Cancer Among People Who Never Smoked. Updated October 15, 2024. Accessed January 13, 2026. https://www.cdc.gov/lung-cancer/nonsmokers/index.html
US Preventive Services Task Force. Recommendation: Lung Cancer: Screening. Published March 9, 2021. Accessed January 13, 2026. https://www.uspreventiveservicestaskforce.org/uspstf/recommendation/lung-cancer-screening
Cizzle Bio, Inc. Lung Cancer, The CIZ1B Biomarker. Accessed January 13, 2026. https://www.cizzlebio.com/lung-cancer-test-ciz1b


















Priscilla Brittine lost family to stomach cancer, then learned she carries a CDH1 mutation. Her decision to undergo preventive surgery revealed early-stage cancer that endoscopy missed, reinforcing why earlier detection tools are urgently needed.